Healing Generational Trauma: Combining Epigenetics and Holistic Healing
Healing Generational Trauma: Combining Epigenetics and Holistic Healing ~ Discover the Power of Integrated Healing!

The journey toward healing generational trauma begins with understanding its profound impact on personal development and familial patterns. Acknowledging the existence of inherited trauma is a pivotal step in breaking the cycle that has, for generations, influenced countless aspects of life and well-being. The significance of this healing process cannot be overstated, as it holds the key to unlocking a future where past pains no longer dictate the dynamics of one's life and relationships. This initiative is not merely about healing oneself but extending that healing back through generations and forward to those yet to come. It's about altering the narrative from one of enduring suffering to one of resilience and transformation.
As you navigate through this article, you will explore the intricate relationship between trauma and DNA and how epigenetic changes in the brain after early childhood abuse can influence not just the individual directly affected but successive generations. We will delve into the science of epigenetics in trauma, uncovering how trauma can be passed down and its implications. The discussion will extend to both conventional and holistic approaches for healing generational trauma, providing a comprehensive understanding that bridges the gap between traditional psychological methodologies and more nuanced, whole-person strategies. By the conclusion, you will be equipped with the knowledge and perspective needed to embark on your journey of healing epigenetic trauma, armed with insights from epigenetics and holistic healing to foster deep, lasting change.
Understanding Multigenerational Trauma
Traumatic experiences manifest in various forms, but certain types have profound, rippling effects across generations. Major traumatic events, such as large-scale disasters or systemic oppression, often impact not only those who directly experience them but also reverberate through their descendants [1]. This phenomenon, known as intergenerational or multigenerational trauma, encompasses the transmission of trauma from survivors to their offspring, potentially affecting multiple aspects of life, including relationships, mental health, and personal identity [1] [2].
Short-term and Long-term Implications
In the short term, descendants may exhibit signs often associated with mental health conditions like depression or PTSD. These can include emotional numbness, difficulty in forming relationships, and a heightened stress response [1]. However, the long-term implications of multigenerational trauma extend further, influencing not just psychological health but also physical well-being. Research shows that stress responses can lead to serious health issues such as heart disease and diabetes [3].
Understanding these traumas requires acknowledging the pervasive and persistent nature of their impact. For instance, children and grandchildren of Holocaust survivors often display distinct emotional and behavioral patterns, which stem from the coping mechanisms developed by their ancestors in response to their experiences [3]. Similarly, families affected by historical oppression may continue to struggle with trust and communication issues, inadvertently passing these challenges down through generations [1].
The key to addressing these deep-seated issues is recognizing the complex interplay between inherited psychological responses and current behaviors. By doing so, you can unravel the threads of past traumas that shape present experiences, paving the way for healing and transformation.
Get your signed copy of Dr. Rick Wallace's 28th book, Healed & Whole!
The Science of Epigenetics in Trauma
Key Concepts in Epigenetics
Epigenetics involves studying how behaviors and the environment can cause changes that affect how genes work without altering the DNA sequence itself. This field examines how certain activities and environmental factors can turn genes "on" and "off," impacting everything from health to susceptibility to diseases [4]. Understanding epigenetics is crucial as it explains how the expression of genes can be influenced by factors such as nutrition, stress, and exposure to toxins [5].
Mechanisms of Epigenetic Changes Due to Trauma
Trauma can lead to epigenetic changes through DNA methylation and histone modification. DNA methylation typically suppresses gene expression and is a common response to traumatic experiences, affecting how genes are expressed without altering the underlying DNA sequence [6]. Histone modifications, which include processes like acetylation and methylation, also play a significant role in gene regulation. These modifications can either condense or relax chromatin, the structure that holds DNA, thereby influencing gene expression by enhancing or reducing transcription [7].
The Role of DNA in Health Outcomes and the Role of Epigenetics
The impact of epigenetics extends beyond immediate health responses to trauma; it also has long-term implications for disease susceptibility and mental health. For instance, epigenetic modifications can influence the development of conditions like PTSD, depression, and even physical illnesses such as heart disease [8]. Epigenetic changes can serve as biomarkers for disease and provide targets for therapeutic interventions. By understanding these mechanisms, mental health professionals can better tailor treatments to the individual, potentially reversing the adverse effects of trauma [5] [9].
These insights into epigenetics enhance our understanding of how trauma affects health across generations and underscore the importance of addressing both genetic and environmental factors in treatment strategies.
Adverse Childhood Experiences (ACEs) and Their Impact
Defining ACEs
Adverse Childhood Experiences (ACEs) encompass a range of traumatic events that occur before the age of 18. These can include exposure to abuse, neglect, and household dysfunction. The impact of ACEs extends beyond immediate emotional distress, influencing long-term mental and physical health [10][11].
Common Types of ACEs
The types of ACEs vary widely but commonly include physical, emotional, and sexual abuse, witnessing domestic violence, and living with family members who struggle with addiction or mental health disorders. Importantly, ACEs also cover aspects like parental separation or incarceration, which can undermine a child’s sense of security and stability [12][13].
Long-term Effects of ACEs
The repercussions of ACEs are profound and far-reaching. Adults who experience ACEs as children are at an increased risk for a variety of conditions, including depression, heart disease, and diabetes. These experiences can also lead to harmful behaviors such as substance abuse and high-risk sexual activities, significantly shortening life expectancy [14][15]. The toxic stress from ACEs can alter brain development and affect how the body responds to stress, impacting everything from immune function to hormonal balance [10][11][13].
Register for the Live Virtual Healed & Whole Event! (Experience a Life-altering Transformation).
Proactive Prevention of ACEs
Preventing ACEs is crucial for breaking the cycle of trauma and promoting healthier, more resilient generations. Strategies include enhancing support for affected families through access to quality childcare and economic support and implementing family-friendly policies in the workplace. Additionally, community programs that promote safe, stable, and nurturing relationships are essential in mitigating the impacts of ACEs [10][16].
Transmission of Trauma Across Generations
Biological Transmission
Generational trauma, also known as transgenerational trauma, involves the transmission of traumatic experiences from one generation to another [17]. This can occur through epigenetic changes, where traumatic experiences lead to modifications in gene expression without altering the DNA sequence itself. Such changes can leave a chemical mark on DNA, influencing how genes are expressed and potentially affecting multiple generations [17][18]. Research indicates that these epigenetic changes can occur due to various traumatic experiences, such as exposure to war, abuse, or natural disasters, and can be passed down from parents to their children [17][18].
Behavioral and Environmental Transmission
In addition to biological factors, generational trauma can also be transmitted through behavioral and environmental pathways. Trauma survivors may parent in ways that expose their children to similar traumatic experiences or create an environment that mirrors the original trauma. This can include patterns of emotional detachment, substance abuse, or other maladaptive behaviors that indirectly affect the children in the household [19]. Furthermore, community and cultural factors can perpetuate trauma, influencing family dynamics and parenting styles over time, thus continuing the cycle of trauma [19][18].
Healing through Trauma Prevention and Intervention
Addressing generational trauma requires a comprehensive approach that includes both prevention and intervention strategies. Trauma-informed prevention programs are essential in breaking the cycle of trauma by addressing both biological and behavioral/environmental factors [20]. These programs can help families develop healthier relationships and reduce the transmission of trauma to future generations. Additionally, intervention strategies should focus on supporting trauma survivors through therapy and community support systems, helping them to cope with and heal from their experiences. By integrating these approaches, it is possible to mitigate the long-term effects of generational trauma and promote resilience in affected individuals and communities [20].
Case Studies of Multigenerational Trauma
Study 1: Examples from War Survivors
The intergenerational transmission of trauma among war veterans and their descendants has been extensively studied. Research suggests a significant association between veterans' war exposure and the psychological characteristics of their offspring, even 40 years after the trauma. The intensity of war exposure, rather than the presence of PTSD in veterans, appears to influence the psychological suffering of their children [21]. This highlights the need for early mental health support for veterans' families, focusing on the intensity of war exposure to mitigate long-term psychological effects.
Study 2: Impact on Indigenous Populations
Indigenous communities in Canada have faced multigenerational trauma, primarily through the Indian Residential School (IRS) system, which aims to assimilate Aboriginal peoples. Studies indicate that descendants of IRS survivors exhibit increased risks of psychological distress, educational challenges, and poorer well-being. These effects are compounded when the familial history of IRS attendance intersects with current stressors, suggesting that IRS trauma accumulates across generations [22]. This case underscores the importance of addressing historical and current traumas in healing interventions.
Study 3: Impact on African American Descendants of Slaves
African Americans have endured centuries of structural racism, starting from chattel slavery to ongoing systemic inequalities. This has resulted in Post Traumatic Slave Syndrome (PTSS), a condition reflecting the multigenerational impact of oppression. Historical trauma among African Americans is linked to higher rates of infant mortality, mental health disorders, and economic disparities. Addressing this requires a trauma-informed approach that recognizes the deep-seated nature of racial trauma and incorporates healing-centered engagement, focusing on collective well-being and interdependence [23][24].
Conventional Approaches to Healing Trauma
Traditional Therapy Methods
Conventional approaches to healing trauma have evolved significantly, with a strong emphasis on trauma-focused therapies. Cognitive Processing Therapy (CPT), Prolonged Exposure Therapy (PE), and Eye Movement Desensitization and Restructuring (EMDR) are recognized as the gold standards in the field. These therapies are designed to address the root causes of trauma by helping you process traumatic memories in a structured, supportive environment. Notably, these treatments often involve 12-16 sessions of intensive, 60-minute therapy that can significantly reduce symptoms of PTSD [25].
Manualized therapy, where a structured guide is employed, has been shown to enhance treatment outcomes. This approach ensures that all critical trauma-related topics are addressed systematically, enhancing adherence to the treatment and the long-term resolution of symptoms [25]. Additionally, emerging therapies like Written Exposure Therapy offer a tactile approach to processing trauma, which can be particularly beneficial for individuals who find traditional verbal therapies challenging [25].
Limitations of Conventional Treatments
Despite the effectiveness of these established therapies, there are notable limitations to conventional approaches. Access to these evidence-based treatments can be significantly hindered by geographical location, socioeconomic status, and the availability of trained professionals. In many regions, especially in low- and middle-income countries, there is a stark lack of access to qualified mental health care providers, which can leave many trauma survivors without the necessary support [26].
Furthermore, the traditional focus of these therapies often does not account for cultural sensitivities, which can affect the treatment's effectiveness across different populations. The need for culturally sensitive treatment options is critical in addressing the diverse impacts of trauma on various communities [26]. Additionally, conventional treatments typically require a considerable time commitment and consistent participation, which can be a barrier for individuals with demanding schedules or those who live in unstable circumstances [25].
Considering these conventional approaches, evaluating the potential benefits and limitations is important to find the most suitable method for your healing journey.
Holistic Healing Approaches
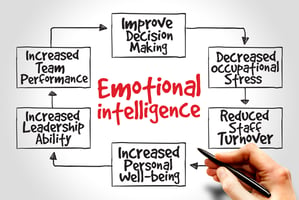
Integrative Therapy
Integrative therapy, in the context of holistic healing, combines multiple therapeutic modalities to treat the whole person—mind, body, and spirit. This approach often includes traditional psychological methods and alternative treatments such as nutrition, yoga, and mindfulness [27]. Integrative therapy supports comprehensive healing and personal growth by addressing various aspects of an individual's life.
Mind-Body Practices
Mind-body practices are essential to holistic healing, focusing on the connection between mental and physical health. Techniques like yoga, meditation, and deep breathing help manage stress and are proven to improve symptoms of PTSD and other stress-related conditions [28] [29]. These practices alleviate psychological distress and enhance overall well-being by boosting self-esteem, increasing pain tolerance, and improving the ability to relax and cope with stressful situations.
Community Support Systems
The role of community and social support is critical in holistic healing approaches. Effective healing from trauma can be significantly supported by relationships with others who understand and share similar experiences. For instance, veterans have shown improved psychological health through communal support and altruistic behaviors, which help reduce feelings of isolation and increase life purpose [30].
Mindfulness and Meditation
Mindfulness and meditation are pivotal in managing trauma-related symptoms by fostering a mindful awareness of the present moment, reducing avoidance, and promoting emotional regulation [31]. Mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT) are particularly effective, offering structured programs that include group sessions and daily practices aimed at reducing symptoms of PTSD and enhancing emotional well-being. Moreover, trauma-informed mindfulness practices adapt these techniques to meet the specific needs of trauma survivors, ensuring a safe and supportive healing environment [32].
The Future of Trauma Healing
Emerging Research
The landscape of trauma healing is witnessing significant advancements, with emerging research focusing on innovative strategies. New treatment options, including psychedelics like MDMA, psilocybin, and ibogaine, alongside procedures like stellate ganglion block (SGB), are showing promising results in preliminary studies [33]. SGB, a procedure involving the injection of a local anesthetic into the neck's nerve cells, has been found effective in treating PTSD, offering a fast-acting solution to those for whom other treatments have failed [33]. This approach is supported by compelling evidence that underscores its safety and efficacy, marking a new era in PTSD treatment that combines speed with reliability [33].
However, these novel treatments also introduce new risks, primarily due to the involvement of underqualified providers or the treatments' experimental nature [33]. As such, it is crucial for individuals seeking these treatments to ensure that providers use the most reliable methods, like ultrasound guidance for SGB, and to verify the provider's experience and patient feedback [33].
Potential Integrative Strategies
Integrative strategies that combine traditional and complementary therapies are gaining traction. Cognitive-behavioral therapy with mindfulness-based practices and somatic interventions like yoga and breathwork are particularly noteworthy [34]. These approaches not only address the psychological aspects of trauma but also its physical manifestations, helping individuals reconnect with their bodies and regulate their nervous systems [34].
Moreover, technology-based interventions such as virtual reality therapy and biofeedback are being explored for their potential to enhance the effectiveness of trauma treatments, providing safe environments for patients to confront and process their traumatic experiences [34]. The AURORA study, a major national research initiative, exemplifies this forward-thinking approach by using advanced tools in genomics and neuroimaging to develop new treatments for trauma survivors [35].
As the field of trauma healing evolves, it is imperative to continue supporting research that seeks to understand and improve the efficacy of both new and integrative treatment modalities. This ongoing research is essential to ensure that the future of trauma healing is both innovative and grounded in evidence-based practices [33][35][34].
Conclusion
Throughout this article, we've embarked on a comprehensive journey exploring the depths of healing generational trauma, intertwining the realms of epigenetics and holistic healing methods. We've delved into the complexities of how trauma is inherited and manifests across generations and highlighted the innovative approaches that hold promise for breaking these cycles of pain. Emphasizing the significant role of traditional and integrative healing modalities, the insights drawn underscore the importance of addressing trauma in a multifaceted manner—considering the individual's biological, psychological, and environmental contexts to foster profound healing and transformation.
In light of these discussions, the path forward calls for a deeper engagement with both established and emerging therapies that embrace the full spectrum of human experience in addressing trauma. By harnessing the potential of integrative healing strategies, there is hope for individuals and communities to reclaim their stories, transforming inherited narratives of suffering into legacies of resilience, strength, and renewal. The journey towards healing is personal and collective, underscoring the shared mission to nurture well-being across generations, and it is this journey that holds the key to unlocking a future where liberation from generational trauma is not just possible but promised.
FAQs
1. Is it possible to heal from epigenetic trauma?
Yes, it is indeed possible to reverse epigenetic trauma. Advances in understanding how our bodies function have shown that epigenetic tags, which may be added due to trauma, can be removed. This is achieved through various psychotherapeutic interventions, allowing for the healing and reversal of epigenetic impacts.
2. What role does epigenetics play in generational trauma?
Epigenetics is critical in understanding generational trauma as it explains how the effects of trauma can be transmitted across generations. It provides insights into how traumatic experiences, like violence and childhood abuse, can affect not only those who directly experience them but also their descendants. This understanding is vital for developing interventions that can break the cycle of trauma.
3. What does epigenetic healing involve?
Epigenetic healing, particularly noted in oncology, involves using chemical and biological agents to encourage abnormally transformed cells to return to normal functioning and differentiation. This approach is promising for treating various conditions by altering epigenetic modifications.
4. How can one heal from generational trauma?
Healing from generational trauma involves several strategies that one can adopt, including:
- Recognizing, acknowledging, and accepting the trauma experienced.
- Engaging in mindfulness and meditation to foster mental clarity and emotional stability.
- Setting personal boundaries to protect emotional well-being.
- Practicing self-care to improve overall health and resilience.
- Communicating openly and seeking support from others who understand or share similar experiences.
References
[1] - https://www.healthline.com/health/mental-health/intergenerational-trauma
[2] - https://www.verywellmind.com/what-is-integenerational-trauma-5211898
[3] - https://www.goodtherapy.org/blog/Understanding_Intergenerational_Trauma/
[4] - https://www.cdc.gov/genomics-and-health/about/epigenetic-impacts-on-health.html
[5] - https://www.verywellmind.com/awareness-of-epigenetics-and-generational-trauma-can-inform-therapy-and-empower-those-struggling-with-their-mental-health-5218280
[6] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9676221/
[7] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6952751/
[8] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6857662/
[9] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4480875/
[10] - https://www.cdc.gov/vitalsigns/aces/index.html
[11] - https://my.clevelandclinic.org/health/symptoms/24875-adverse-childhood-experiences-ace
[12] - https://www.cdc.gov/aces/about/index.html
[13] - https://www.cdc.gov/aces/media/pdfs/ACEs-Strategic-Plan_Final_508.pdf
[14] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4617302/
[15] - https://www.ctipp.org/post/aces-prevention-saves-lives
[16] - https://osg.ca.gov/wp-content/uploads/sites/266/2020/12/Part-II-2.-Primary-and-Secondary-Prevention-Strategies-in-Healthcare.pdf
[17] - https://www.sandstonecare.com/blog/generational-trauma/
[18] - https://www.makinwellness.com/stop-generational-trauma/
[19] - https://www.transformationsnetwork.com/post/breaking-generational-trauma
[20] - https://www.healthcentral.com/condition/post-traumatic-stress-disorder/epigenetics-trauma
[21] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6688296/
[22] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4232330/
[23] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8352535/
[24] - https://www.health.state.mn.us/communities/equity/projects/infantmortality/session2.2.pdf
[25] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8672952/
[26] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5496089/
[27] - https://www.theholisticcounseling.center/blog/what-is-holistic-counseling
[28] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3668544/
[29] - https://www.newportinstitute.com/resources/mental-health/the-mind-body-connection/
[30] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9534006/
[31] - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5747539/
[32] - https://psychcentral.com/health/trauma-informed-mindfulness
[33] - https://www.rti.org/insights/new-ptsd-treatments-offer-hope-with-caution
[34] - https://www.sciencedaily.com/releases/2024/02/240205165831.htm
[35] - https://www.med.unc.edu/itr/aurora-study/

-1.png?width=497&height=417&name=Healed%20%26%20Whole%20~%20The%20Event%20(1)-1.png)